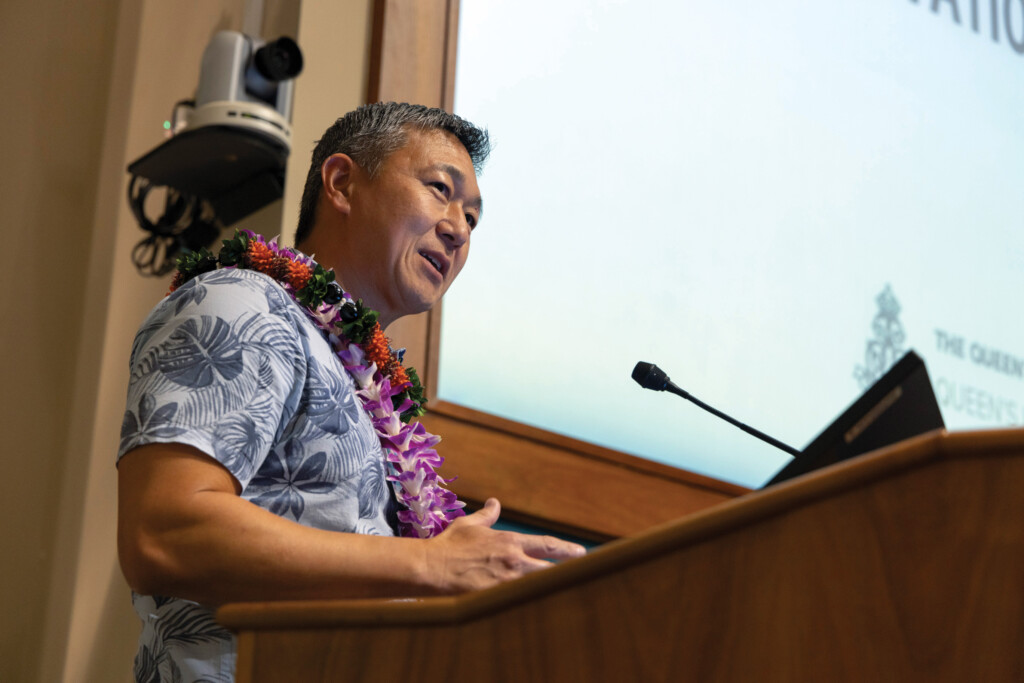
Meet Jason Chang, the New CEO of Queen’s
The leader of Hawai‘i’s largest health-care system brings fresh ideas for expanding services statewide while stabilizing the financials.

Jason Chang served for nine years as chief operating officer, executive VP and then president at the Queen’s Health Systems.
Then on July 12, Jenai Wall, chair of the system’s board of trustees, announced that Chang would take over as CEO. Immediately.
Jill Hoggard Green, hired as CEO in 2019, was out and Chang was in. “The board extends its heartfelt mahalo to Jill for her dedicated service and leadership over the last five years,” Wall said in a written message to the Queen’s leadership team that did not explain the abrupt transition.
In the weeks after Chang’s responsibilities changed overnight, he had few openings on his calendar and twice had to reschedule my interview. But he smiled frequently and showed no signs of stress when I eventually sat with him in his old office (he had not yet moved into the CEO’s office), a room lined on one side with pictures of his wife and three children and on another with a large picture of a beautiful Kaua‘i waterfall.
Though he was born in Fresno and spent his early career in California and Texas, Hawai‘i is now home for him and his family. “We fell in love with Hawai‘i. God willing, I want to retire here,” he says.
Following is a condensed, lightly edited version of my exclusive 40-minute interview with him.
Q: What are your short-term and long-term goals for the Queen’s Health Systems? Let’s start with short term.
I think the most immediate thing is we need to stabilize our financials. Not just here, but health care around the nation. The last two years have been really challenging. Costs have gone up with inflation. There’s wage increases among our regular staff and our physician staff. I can’t just raise prices. It’s basically fixed pricing.
So you have to figure out how you can be more creative within. And the needs for access to care for the most vulnerable patients, patients with behavioral issues or homelessness issues – that’s not slowing down. In fact, it’s actually increasing. So how do you take care of patients that need us the most, yet still be financially sustainable? There’s a very fine balance and that margin that used to be there, it’s gotten tighter.
Sustainability is the first thing. Got to take care of our people, that’s the second-most important thing. Our staff. We have really loyal people here. If you’ve ever walked through the hallways and talked to any one of them, you’ll feel that aura of living and working for the queen. The values are aligned.
That’s special. I’ve worked in California and Texas and you don’t get that same feeling. People are here to take care of their community, people are here because of the mission. So we have to make sure they feel valued and know there’s a future for them at Queen’s.
We just celebrated 165 years this year and largely our mission hasn’t changed. Our job is to fulfill the intent of Queen Emma and King Kamehameha IV: to provide in perpetuity, quality health care services to improve the well-being of Native Hawaiians and all the people of Hawai‘i.
One hundred and sixty-five years ago, that’s what they set out as the mission, when they saw 70% of the native-born population dying over their lifetime because of disease. And so they went door to door to raise funds, founded a hospital right here on this campus, the Manamana property. And that’s why there’s this aura when you walk across this campus – that legacy is now our job.
Q: What about long-term goals, maybe five, 10 years from now?
I think that there’s a lot of opportunity for Queen’s to expand our reach. We have hospitals on O‘ahu, a hospital on Moloka‘i and a hospital on the Big Island. And now we have a medical group that’s dispersed around, but mostly in the same places.
We’re not on Kaua‘i or Maui, we don’t have a presence over all the Big Island. There are rural communities where people are not getting care, preventive care, cancer care, cardiac care.
Long term, I think we can use technology, we can expand our footprint, we can build culturally sensitive care that communities around the state embrace, so we become the true health care system for the entire state of Hawai‘i.
Q: One project you recently launched was the Aukahi Center, which collects data to help manage patients throughout the Queen’s Health Systems.
That is a special project to me. The name Aukahi is fitting because it means water rolling down a mountainside, converging and flowing into a larger stream. I feel the data that’s flowing through this command center is exactly that. Information about patients in our hospitals, patients that need to be transferred, wanting to see a doctor or get an MRI. Aukahi is like an air traffic control center. We can oversee things that we’ve never been able to see in real time before.
Say a patient needs an MRI, a cardiac consult and physical therapy before they can go home that day; we can see that and assign a cardiologist, then get that patient into an MRI, and then get that physical therapist there so the patient doesn’t languish in the hospital longer than they need to. It helps move people through the system.

Chang at the Aukahi Center, which was one of the projects he helped launch before becoming CEO. It is designed to help manage patients more effectively by using data collected throughout the Queen’s Health Systems.
We can do other things like remote patient monitoring. We can see if a patient’s diabetes is becoming uncontrolled, call them and say, “You need to see your doctor,” before they end up in the emergency department. Aukahi is the first of its kind in Hawai‘i.
I think the piece that will add to it is the ability to dispatch the state’s helicopter system – getting patients from a Neighbor Island to a destination they need as expeditiously as possible.
Q: Queen’s is taking over the dispatch function of Medevac helicopters on Maui this September, but Queen’s is not on Maui. Why take on that contract?
It’s us dipping our toe into dispatching the helicopter. There’s one helicopter now and we will learn how to dispatch this helicopter safely – getting a patient from Maui to the next destination they need. It could be within the Queen’s Systems, it could be to a different system. Essentially, we’re doing something good for everybody.
There will be more helicopters in the future, but let’s start with one, and then it’ll grow to three, and then we’ll go to five and seven. That’s the way we’re partnering with EMS to get patients to and from places as quickly as possible.
Now, if you get into a car accident on the Big Island, the ambulance picks you up, takes you to the nearest hospital, they stabilize you, put you back in the ambulance, drive you to the airport, fly you to O‘ahu. You get picked up by the ambulance, they drive you here to The Queen’s Medical Center. What if the helicopter picks you up at the crash site and flies you here? Then you’ve cut three, four hours.
For patients that have heart attacks, strokes, trauma, this could be the difference between life and death or not having quality of life.
Q: Let’s talk about one of your biggest challenges: staffing. It’s always been hard for health care to fully staff, then the pandemic and the retirement of baby boomers made it harder.
One of our biggest challenges over the last three, four years has been recruitment. And it’s not just nursing. But we’re trying to partner better with universities, community colleges, high schools, get people interested in health care, show them that you don’t just have doctors and nurses in a hospital. There are hundreds of different jobs we need.
What we haven’t done in the past is hire them without any experience. In the past, if you are clinical especially, we wanted you to get three years of experience. The risk is that, nurses in particular, go to the mainland and never come back. So let’s give them a job. Provide protected time for them to train, get oriented, be safe, and then let them fly and give them career opportunities to grow.
If you want to be a cardiac nurse or ICU nurse or surgical nurse, they can see the path within the organization. We’ll take that journey together.
Security is another area having challenges finding qualified people. But you come in with us, get a few years under your belt and there’s a career ladder for you to step up and get more competency. Maybe your aspiration is HPD or with Honolulu Fire. This could be that career ladder to you, maybe not just within the organization, but helping provide the security we need today.
Q: What are your other challenges?
Access. What we’re living through today, we didn’t anticipate. We knew there was going to be more patients, more need for diagnostic imaging and doctors, but the pandemic accelerated it. Now we are seeing our hospital census in the range of 102 to 105% of capacity. And the patients are sicker.
We need to figure out ways we can use technology to be really smart about how to get a patient through the acute part of the health care system so they can transition to post-acute. We have partners in the community that they can move to, because as the quaternary facility (where patients receive the most advanced and specialized level of medicine), we need to be ready for the sickest patients.
Our community hospitals are also running full. Queen’s Medical Center-West O‘ahu is now seeing nearly 185, 186 patients a day in the emergency department. It’s just a hair behind the Queen’s Medical Center-Manamana (the original Punchbowl Street facility), which is the trauma level-one emergency department.
It’s a big challenge. Our teams have been fantastic. You walk in, you would never know that they were under such stress. But we know they are. So how can we help alleviate the working environment challenges?
Step number one includes building more facilities. West is going to add 48 beds to their emergency department. We’re expanding the emergency department here at Manamana. That helps relieve some of that pressure.
Making sure everybody on the team knows the path we’re on. Make sure they know, “This is the plan and we’re going to walk this plan arm in arm.” Then give people an opportunity to have a voice. We’re not talking about unilateral decisions; we want open-door policies where people can come in and talk about the things they think should happen.
I’ve always believed that the best guidance comes from the people working on the front line; they know what’s happening, they can tell the temperature of the organization. And if they feel safe enough to tell it to you, all I have to do is listen. So you’ve got to have a great relationship with the people doing the work. The best part of my day is walking the halls and talking to people.
Q: When you look back at your career, what experiences especially helped you prepare for this job as CEO of Queen’s?
I’ve had great mentors over my career, people who took time to help me grow and learn how to succeed in the hospital industry.
One amazing piece of advice early in my career was that I needed to get experience in the for-profit world. So I went from a Catholic hospital to a for-profit, publicly traded health system in Texas and worked there for several years before I came to Queen’s.
It’s very different than the not-for-profit health care world. It’s predicated on making a margin. You have shareholders, calls every quarter. I learned to advocate for the things that are important to that health system, to that hospital you’re running, which is an asset of the corporation. And if you sacrifice patient experience, patient access, trust in the community, then you diminish the value of that asset for that corporation. In that for-profit world, you learn to balance advocating for the services the community needs yet have enough margin for the parent corporation. It’s a very challenging environment – pressure cooker every day.
Coming to Queen’s allows me to use that business acumen and to be a good steward of resources, but at the same time, embrace the mission that Queen’s has been leading for 165 years. It gives me personal fulfillment, being able to do things for the community, plant roots and be here for the rest of my career, God willing.
Q: What’s one other thing happening at Queen’s?
We’re looking at populations that are very vulnerable and seeking creative ways to care for them. Behavioral health is a good example. And we’ve learned we can’t do that by ourselves. Building partnerships with like-minded organizations has been tremendously fruitful.
Q: Who are some of those partners?
Kamehameha Schools, Lili‘uokalani Trust, IHS (the Institute for Human Services), St. Francis Healthcare System. There are so many out there. And the more we partner, I think the better health care is going to be.