Hawaii Business Environmental Report: Mosquitoes

Mosquitoes have already caused a dengue fever outbreak in Hawaii. Zika and other mosquito-borne diseases may be close behind. Here’s what scientists are doing and what you should do.
For most of Kepa Police’s life, mosquitoes were minor annoyances, simply to be swatted away. Then, just before Christmas, the 21-year old contracted dengue fever.
“All I could do was lie down and space out for 10 days straight,” says the Hawaii Island resident. Five days of a high fever, intense chills, pain in his bones, a raging headache and nausea were followed by a full body rash as painful as a bad sunburn.
“I can’t imagine being any sicker than I was then,” he says.
Mosquito-borne diseases kill 1 million people a year globally, debilitating hundreds of millions more. Dengue fever, the fastest-growing mosquito-borne disease in the world, affects 400 million people every year and kills 25,000. The Zika virus is, according to the World Health Organization, “spreading explosively” across Latin America and has gained a foothold in American Samoa.
“WE SHOULDN’T LOOK AT THIS AS JUST A BIG ISLAND PROBLEM. WE SHOULD LOOK AT THIS AS A STATEWIDE PROBLEM. THIS SHOULD BE AN ALL-HANDS-ON-DECK MOMENT FOR HAWAII.”
-JOSH GREEN
PHYSICIAN AND STATE SENATOR
Since September 2015, there have been 263 confirmed cases of dengue on Hawaii Island and five cases of Zika brought to the state by people who contracted it elsewhere. Although these numbers do not indicate that either will become endemic, Hawaii’s tropical climate and popularity as a travel destination make it easy for mosquito-borne diseases to spread.
What can we do to combat the most dangerous animal known to humans? Scientists, health officials and community members weigh in on what we need to know and do.
AEDES AEGYPTI THRIVES WHERE HUMANS LIVE
We don’t need to look far for the mosquito that transmits dengue and Zika. It has moved in with us.
“Aedes aegypti is a domestic mosquito, one that we find in human dwellings. That’s what makes it a better vector than the other dengue transmitter, Aedes albopictus. It lives indoors right where the people are, and never moves from that habitat,” explains Dennis A. LaPointe, a research ecologist focused on mosquito biology at the USGS Pacific Island Ecosystems Research Center.
Within the state, Aedes aegypti is currently found only on Hawaii Island. Globally, however, it has spread across the southern U.S. as well as in Latin America and the Caribbean.
Unlike other female mosquitoes that feed on a combination of animal blood and flowers, Aedes aegypti females have evolved to feed exclusively on human blood. They use some to maintain themselves and some to reproduce, biting more often than other mosquitoes, thus making disease transmission more likely.
“They’ve adapted in such a way that they never have to look far for their host,” LaPointe adds.

Mosquito larvae raised by the company Oxitec have a “self-limiting gene.” When males are released and mate with wild females, their eggs hatch but the larvae die before they become disease-transmitting adults.
Photo Courtesy: Oxitec
Unlike other mosquitoes, which require dirty, organically rich water for their eggs to survive, Aedes aegypti thrive in small amounts of clean water, such as rain in discarded tires, soda cans, curled leaves, pet bowls or even bottle caps.
“These mosquitoes can breed in as little as a teaspoon of water. If you have a little tray or planter or area that’s shaded, and a little bit of water that can persist, that’s a potential breeding site, says Sarah Park, state epidemiologist and chief of the Disease Outbreak Control Division at the Hawaii Department of Health.
TRADITIONAL METHODS HAVE LIMITS
Although insecticides have been used for decades, mosquitoes infect more people every year. Insects become resistant to some pesticides and people also resist them because of health concerns.
Aerial spraying can be useful in emergencies, but only affects adult insects. “Four days later you have the same number of mosquitoes with a new larvae hatch. Unless you’re dropping malathion (a common pesticide) every few days, you’re not doing much good,” says David M. Morens, senior advisor to the director at the National Institute of Allergy and Infectious Diseases.

A researcher at Monash University in Australia, who is studying Wolbachia, reaches inside a case filled with mosquitoes.
Photo Courtesy: Eliminate Dengue
Furthermore, because Aedes aegypti live inside with us, reaching them can be a challenge. “To control the mosquito, a public health authority has to have access to everyone’s home,” says Oxitec CEO Hadyn Parry. “In a modern society, that’s not only impractical, but also unacceptable.”
Larvicides, such as tablets applied to water, stop the next generation. But it can be difficult to find all the tiny places where they breed.
“People are oftentimes well intentioned but may not realize some things hold water,” says Kacey C. Ernst, associate professor of epidemiology at the University of Arizona. “Even if you could completely clear a yard, there may be something that you can’t see visually, and that can become a breeding site.”
INDIVIDUAL INITIATIVES MAKE A DIFFERENCE
Easter Aquino-Schorle used to let mosquitoes around her Hawaiian Paradise Park home limit her daily life. “I would avoid going out in the morning and evening. I’m one of those people – even if I were in a crowd of thousands, one mosquito would find me.”
That was before she learned how to make mosquito traps. Since she started making them in January, she estimates she has killed about 600 eggs weekly. “I used to get bitten several times a day and, now, it’s down to just one or two times a week. Now I can go outside whenever I want.”
Springstar, a Seattle company, offers ready-made traps, which mimic the mosquitoes’ breeding sites (springstar.net).
Puna resident and retired scientist Van Eden runs workshops to teach people how to make their own. “The trap has a landing pad where the mosquito will end up to lay her eggs. You put poison on it, and when she lands on it, she gets a lethal dose. Then, to make sure none of the eggs produce mosquitoes, you put larvicide in the water.
“None of this is hard to do,” says Eden.
Officials and community members are also urging residents to clean the areas around their homes, paying special attention to old appliances, discarded tires, unused cars and other things that can become breeding sites.
“We’ve been working with property owners with issues like standing water. These might be due to natural geographical features or manmade things like catchment systems. Going forward, we want to remove all opportunities for vectors to thrive,” says Hawaii County Civil Defense director Darryl Oliveira.
TURNING MOSQUITO BIOLOGY AGAINST ITSELF
Oxitec CEO Hadyn Parry believes Aedes aegypti, what he calls “public enemy No. 1,” can be permanently eradicated.
His company, based in the United Kingdom, has developed genetically modified male Aedes aegypti with a “self-limiting gene.” When these males are released and mate with wild females, their eggs hatch but the larvae die within a few days, before they become disease-transmitting and breeding adults. And the larvae compete with viable larvae for food during their brief lives.
“Our inspiration is using mosquito biology against itself,” says Parry.
Trials have been conducted in Cayman, Panama and Brazil, and, in one case, researchers observed a 99 percent decrease in the Aedes aegypti population.
Parry says that, although some may have reservations about the idea of genetic modification, their mosquitoes pose no harm to the environment or other organisms. “The self-limiting gene is not toxic or allergenic. It just effectively stops the insect’s growth. If a bat comes along and eats one of our insects, they get a bit of fat and protein just like a normal mosquito.
“THESE MOSQUITOES CAN BREED IN AS LITTLE AS A TEASPOON OF WATER.”
-SARAH PARK
STATE EPIDEMIOLOGIST, TALKING ABOUT THE SPECIES AEDES AEGYPTI

Mosquitoes with Wolbachia are released during a test in Yogyakarta, Indonesia in 2014. The Wolbachia bacteria is intended to render mosquitoes incapable of transmitting diseases to humans.
Photo Courtesy: Eliminate Dengue
“Furthermore,” Parry continues, “since the larvae die, it’s a genetic dead end. There is no persistence in the environment. From a safety of environment point of view, this is leaps ahead of insecticides.”
Another technique is to sterilize the males by exposing them to gamma irradiation. In fact, the International Atomic Energy Agency has been developing sterile fruit flies, tse tse flies, screw worms and moths for several decades, according to Peter A. Follett, research entymologist at the U.S. Department of Agriculture Pacific Basin Agricultural Research Center.
BACTERIA OFFER NATURAL SOLUTIONS
Instead of focusing on sterility, Eliminate Dengue, a nonprofit based in Australia, uses a natural bacteria called Wolbachia (which is present in up to 60 percent of all insects) to block viruses within the mosquitoes themselves.
“Research to date suggests that Wolbachia can boost the natural immune system of the mosquito, which makes it harder for the mosquito to support infections like dengue and Zika. If the mosquito can’t get infected, then it can’t transmit it to humans,” explains program lead Scott O’Neill.
Because Wolbachia does not naturally occur in Aedes aegypti, the bacteria come from fruit flies and are injected into the mosquito eggs. Female Aedes aegypti with Wolbachia are then released into the wild. Once they mate, they pass the bacteria to their eggs. The goal is to sustain high levels of Wolbachia in wild mosquito populations, as the bacteria are inherited from generation to generation. Thus, unlike other approaches, the goal is not to eliminate mosquitoes, but to eliminate their ability to transmit disease.
“Yes, the mosquitoes will still bite and make you itchy, but they won’t make you sick,” says Shane Fairlie, communications and engagement manager.
Scott says they are very encouraged by their results, and are planning their first large-scale citywide trial in Indonesia this year. “Long-term monitoring in our international project sites has shown Wolbachia is sustaining itself at high levels in the majority of these sites up to five years after application. In areas where mosquito populations have high levels of Wolbachia, we haven’t seen any significant local transmission of dengue.”
HAWAII AT THE FOREFRONT
Organizations in Hawaii are also playing leading roles in the global effort to fight mosquito-borne diseases. Hawaii Biotech, established in 1982, specializes in vaccines for tropical diseases, as well as drugs to block bacteria, such as anthrax, that can be used for bioterrorism.
Instead of using live viruses to make vaccines, they work with molecular biology to create proteins that mimic the viral proteins. “This is a very high-tech form of biotechnology. We’ve chosen this approach because the proteins themselves are very safe, and it’s very easy for us to do the work without a lot of precautions, since we’re not using anything infectious,” says president and CEO Elliot Parks.
Hawaii Biotech has developed a variety of vaccine candidates, including ones for West Nile, tick-borne flaviviruses, Crimean-Congo hemorrhagic fever virus and chikungunya.
A few years ago, Hawaii Biotech sold its early stage dengue vaccine candidate to Merck, the largest vaccine company in the world, where it continues to be developed. They are now working on a dengue vaccine to protect military personnel in tropical or subtropical regions, where immediate and complete immunity is critical.
Over the last few months, Hawaii Biotech has also turned its attention to developing a vaccine for the most talked-about virus today. “Zika is in the same family of viruses as dengue and West Nile. The fact that we’ve taken two of the three of these into clinical trials gives us a leg up,” says Parks.
Hawaii is also home to one of only a small number of state labs in the U.S. where blood specimens can be tested for mosquito-borne diseases.
“As late as 2011, we didn’t have the diagnostic capacity in the state for dengue. We had to send everything to the CDC Puerto Rico lab, which added much more complexity and time,” says state epidemiologist Sarah Park.
“We can now test for all three of these threats – dengue, Zika and chikungunya. We’re only one of nine public health labs outside of the CDC that have this kind of capacity in the U.S.,” says Park.
The state lab not only handles cases within Hawaii, but throughout the Pacific. “There are not a lot of lab-testing capabilities in these small island nations and U.S. territories. We’ve become kind of a big brother to these jurisdictions,” says A. Christian Whelen, administrator for the Hawaii Department of Health’s State Laboratories Division.
The lab is thus often the first to detect viruses in the region: for instance, in 2014, it discovered chikungunya in American Samoa. More recently, it confirmed Zika is circulating there. Many people travel between the Pacific islands and Hawaii, so Whelen and his team pay close attention to these cases.
“Knowing what’s happening in those communities helps us prepare for what may impact Hawaii,” he says.
INFORMATION MUST SPREAD SWIFTLY AND WIDELY
Karen Anderson, a resident of Captain Cook on Hawaii Island, founded the Hawaii Dengue Fever Awareness Facebook page for people to discuss the outbreak. With over 1,500 members, the group shares information on vector control, new cases, trapping techniques and public areas that require cleanup.
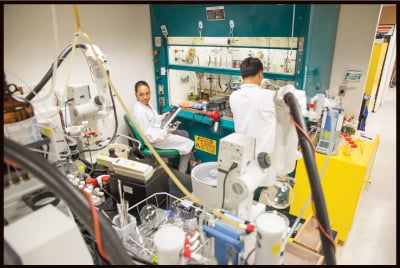
One of Hawaii Biotech’s specialties is vaccines for tropical diseases, and it has already developed a variety of vaccine candidates, including one for dengue. It is now working on a Zika vaccine. Above is the company’s temporary lab on Honolulu’s Young Street.
Evident in the posts, however, are people’s frustration over the state’s response. “People outreach has been really poor in terms of information dissemination. Back in December, the CDC came out and issued its assessment that the state’s public communication capacity was woefully inadequate,” says Anderson.
“We need more press conferences, panels, discussions and Q&A’s online. People need to know how serious it is. So many people here know there’s a dengue outbreak, but don’t know anything about the virus.”
Cutbacks in 2009 reduced the state’s vector-control program to a third of what it was. “Ideally we’d have more capacity on the vector side,” admits state epidemiologist Sarah Park. “A good vector-control program would include a lot of field assessments, public health education with stakeholders on mosquito prevention and surveys to understand where mosquitoes tend to breed and where they are likely to be.”
Many of those interviewed for this article praised the Department of Health’s successful response to the 2001 dengue outbreak on Maui as a worthy model. Bruce S. Anderson, now administrator for the Division of Aquatic Resources, ran the Department of Health then. He describes a more urgent response led by the DOH, backed by more than 80 vector-control staff. There was an aggressive media campaign, including TV spots, and press conferences were held daily. Tens of thousands of brochures were sent to homeowners and passed out at the airport. Officials went door to door.
“We sent our staff from the Health Department out on weekends, and there were literally thousands of people talking to residents about the importance of eliminating potential mosquito-breeding areas,” Anderson says. There were 122 confirmed cases, less than half of the latest outbreak.
THINK AND ACT LOCAL
Bill Cullum, who works on a farm in Captain Cook, came down with dengue symptoms just before Thanksgiving. Once he was tested, it took over two weeks to get his results. “The procedure was unclear, and there was so much back and forth between the physicians and the DOH. Each place told me I had to call the other one to get my results.”
Since testing for dengue can only be done at the state lab on Oahu, the fastest turnaround for Neighbor Island residents is around five days. However, as Cullum’s experience demonstrates, administrative hiccups, weekend closures and the logistics of sending specimens to Oahu can all create delays. By the time results arrive, people may no longer be infectious.
“We had pushed to get testing to be moved to the Big Island. All it requires is a small room, but the DOH didn’t want to move it. That’s how you get a handle on the epidemic. If we start having cases of Zika, we are going to need to be much more proactive in isolating those cases so people aren’t moving around and spreading it,” says state Rep. Richard Creagan, a physician and former bioterrorism preparedness epidemiologist for the state Department of Health.
Creagan points to another local concern that may not be well understood outside of Hawaii Island – the dependence on catchment. “What people in Oahu don’t appreciate is how dependent we are on rainwater. Twenty-thousand homes are on catchment. Catchment tanks are potential breeding areas for mosquitoes, and most people don’t maintain their tanks the way they ideally should. That’s not something the Health Department has wrapped its head around yet.”
Another issue is the reluctance to seek help, say, when you do not have health insurance or gas money to get to a clinic. “You can go to the ER, but people are afraid they will get slapped with a big bill, won’t get tested and will just sit there and suffer,” says Hawaiian Paradise Park resident Kealoha Tam, who says she knows several people who exhibited dengue-like symptoms, but did not seek medical help.
That’s why state senator and physician Josh Green believes the confirmed number of dengue cases underreports the problem. “We knew large numbers had dengue who didn’t get tested. Thank goodness none were life threatening, but, at the same time, it means we have an incomplete assessment of where dengue and mosquitoes are clustered.”
Both Green and Creagan have proposed mobile medical units, in-home visits and other services so people do not have to travel when they are sick.
Tourism numbers rose early this year, indicating the dengue outbreak has not affected the economy, but the reality for small businesses in dengue hot spots is less rosy.
“Local businesses are saying they have lost two seasons of tourists. Some South Kona areas, where beaches were closed, have been having a rough season,” says Green.
What Hawaii Island officials emphasize is the importance of understanding local realities, rather than using an Oahu-centric lens. “Because people in charge don’t live on the Big Island, they don’t have a feeling for what goes on here,” says Creagan. “They don’t understand how it started, and how it’s spreading. They would if they were based here.
WE MUST REMAIN VIGILANT
As of March, the numbers of new dengue cases has slowed considerably, and there’s no evidence that Zika is being transmitted within the state. Nonetheless, the scientists, health officials and community members interviewed for this piece all stress we should not become complacent
David M. Morens, senior advisor to the director at the National Institute of Allergy and Infectious Diseases, worked for 17 years in the epidemiology department at UH Manoa, heading a research lab with a focus on dengue and Zika. “One of the lessons learned is that, in a tropical area like Hawaii, the setup for having an epidemic is always going to be there until all the mosquitoes are eradicated. People like me think of it as a recurrent accident waiting to happen.”
For the long term, global climate change may mean more mosquitoes in more places. “There are studies that show malaria is present in n Africa at higher elevations than it used to be. Mosquitoes are also surviving at higher elevations in Central America as well,” says Korine Kolivras, associate professor in the geography department at Virginia Tech.
“Shifting patterns of rainfall could be important. And everything reproduces more quickly at warmer temperatures,” she adds.
Since the Aedes aegypti eggs can withstand drought for a year or more, fewer mosquitoes during a dry season does not mean they are gone for good. “If we don’t do anything and we have the kind of rainy season we had last year in Kona, then we can forget about it. It’s a lost cause,” says Karen Anderson, founder of the Hawaii Dengue Fever Awareness Facebook page.
Hawaii’s popularity with tourists increases the likelihood of disease transmission. “This is a travel hub. And we have these environmental and recreational facilities that are prime places for harboring and sustaining mosquitoes. We need to raise the level of awareness of how vulnerable we really are,” says Hawaii County Civil Defense director Darryl Oliveira.
Although the recent dengue outbreak has been confined to Hawaii Island, state senator Josh Green urges everyone who thinks this is not their problem, to think again.
“If we get unlucky, and there’s an outbreak in a main tourist area like Waikiki, we could see a 20 percent decline in tourism dollars. That would be devastating to our tax base, which provides for public safety, education and hospitals,” says Green.
“We shouldn’t look at this as just a Big Island problem. We should look at this as a statewide problem. This should be an all-hands-on-deck moment for Hawaii.”
SHORT ANSWERS TO BIG QUESTIONS
What are dengue’s symptoms?
A high fever, severe headache, severe pain behind the eyes, joint pain, muscle and bone pain, rash, and mild bleeding such as in the nose or gums. Younger children and those with their first dengue infection may have milder symptoms.
What are Zika’s symptoms?
Symptoms can be similar to dengue. The most common include fever, rash, joint pain, conjunctivitis (red eyes), muscle pain and headache. Most people, however, may not exhibit any symptoms.
In April, scientists at the U.S. Centers for Disease Control and Prevention said they had conclusively linked the Zika virus with severe fetal brain defects, including microcephaly, a birth defect in which a baby’s head is significantly smaller than expected, often due to abnormal brain development during pregnancy. In Brazil, health authorities have also observed that Zika infections coincide with an increase in Guillain-Barré syndrome, a sickness of the nervous system than can lead to paralysis.
How are dengue and Zika spread?
Both are transmitted to people by the bite of an infected Aedes mosquito. Dengue cannot be spread directly from person to person.
Zika, however, can be spread from an infected mother to her fetus or to her newborn around the time of birth. Zika can also be sexually transmitted through semen from infected males to females. There are still many unknowns, however, including whether a woman can pass the virus to a man through sex.
How are dengue and Zika treated?
There is no specialized medication for either. People who exhibit symptoms should rest, drink plenty of fluids, and use pain relievers with acetaminophen while avoiding those containing aspirin, which could worsen bleeding. Most important, consult a physician.
Is there a vaccine?
No vaccine is available in the U.S. to prevent either, although there is a dengue vaccine registered for use in dengue endemic areas of Mexico, the Philippines and Brazil.
How long is someone infectious?
During the incubation period, large amounts of the virus are present in a person’s blood. That’s when an uninfected mosquito can pick up viruses that can be transferred to other humans.
The incubation period for dengue is typically four to seven days after the infectious mosquito bite. The incubation period for Zika is about three to 12 days after the bite.
If I’ve gotten it once, does that mean I’m immune forever?
There are four strains of dengue fever. If you have gotten dengue fever once, you have immunity only for that strain. Evidence suggests an increased risk of developing severe dengue if you are exposed to a different strain.
It is suspected that, once you get Zika, you have lifelong immunity. However, more research needs to be done.
On Feb. 12, Gov. David Ige declared a state of emergency to prevent the spread of mosquito-borne diseases. What does this mean?
That is a preventive measure to guard against dengue, Zika and other diseases. It gives the government access to the state’s Major Disaster Fund and the option of waiving certain laws and regulations to expedite a response if needed. It also paves the way for federal assistance if the state exhausts its designated resources.
The state of emergency does not mean there are any travel restrictions to Hawaii.
What areas have been affected by the dengue outbreak?
At this issue’s press deadline, the state Department of Health said the current risk areas for dengue were all on Hawaii Island:
• Moderate risk: Milolii
• Some risk: Kailua-Kona, Captain Cook, Volcano
This shortcut takes you to a regularly updated map of risk areas: tinyurl.com/denguemap.
What should I do if I’m in those areas?
• When outdoors, use mosquito repellents, and wear long-sleeve shirts and long pants tucked into socks.
• When indoors, use air conditioning if available.
• Make sure window and door screens are secure and free of holes.
• If you have symptoms of dengue or Zika, seek a medical professional immediately.






